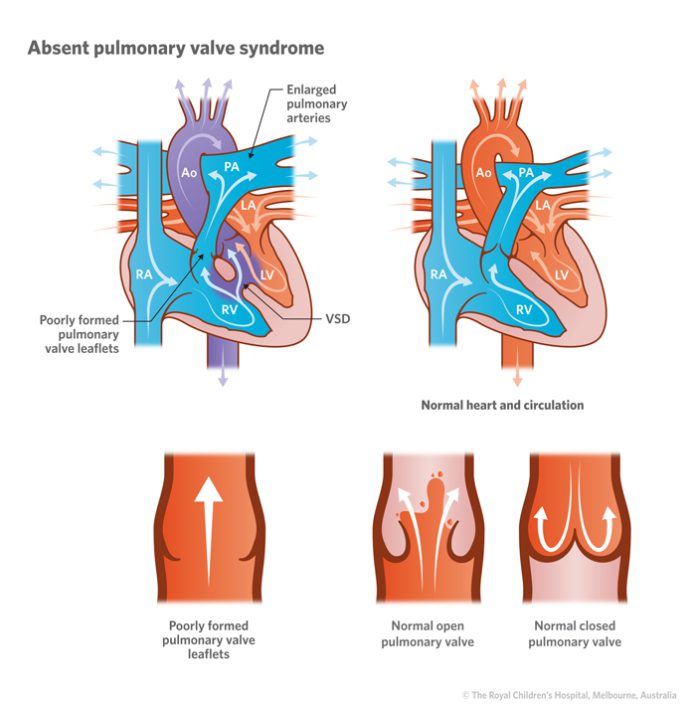
Mencoret.com – An absent pulmonary valve is an anomaly of the heart that causes a shortened ejection fraction. This condition is often diagnosed during fetal life and is caused by abnormalities of the pulmonary valve. A prospectively acquired computerized database of 18,308 pregnancies revealed cases with absent pulmonary valve syndrome. Of these cases, 90% were associated with a ventricular septal defect, a pulmonary artery branch diameter above normal, an arterial duct, and chromosome 22q11 deletion.
These disorders can lead to varying degrees of pulmonary stenosis and regurgitation
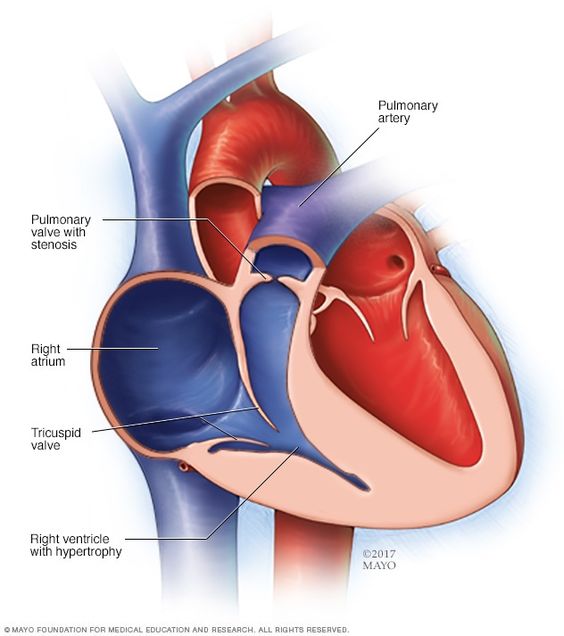
The pulmonary valve is missing in approximately 5% of patients with tetralogy of Fallot. This disorder can cause varying degrees of pulmonary stenosis and regurgitation. Absent pulmonary valve syndrome often occurs with other heart defects, such as tetralogy of Fallot. However, if this condition is present in a neonate, homograft replacement is necessary to restore normal respiratory function.
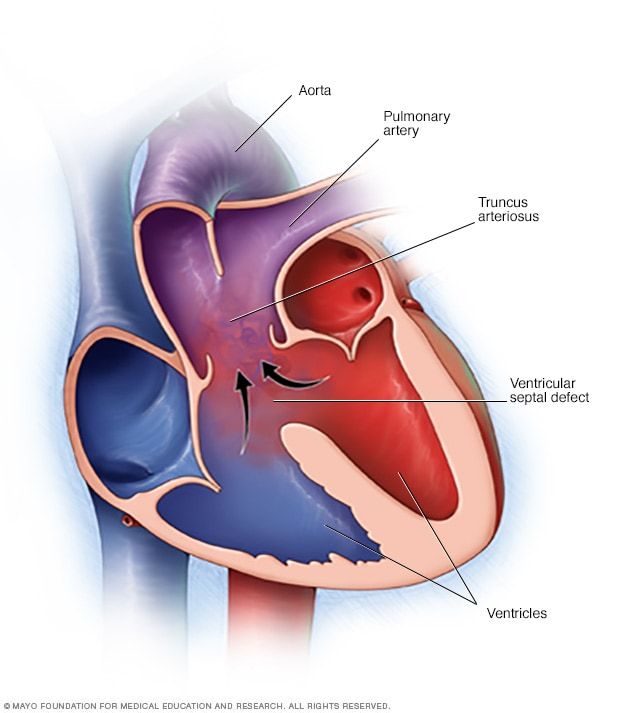
An absent pulmonary valve is the result of a rare congenital cardiac defect. This disorder results in an abnormally thin pulmonary valve with rudimentary leaflet tissue. It is often associated with severe dilatation of the pulmonary trunk and concomitant stenosis. It can also cause serious respiratory compromise and lead to chronic obstructive lung disease. This rare condition is associated with significant perinatal mortality.
Common Fallot or Non-Fallot features
The first known case of APVS was described in 18472. Most APVS cases belong to either the Fallot type or the Non-Fallot type. Both types have common features: an absent or rudimentary pulmonary valve, a dilated main pulmonary artery, and dilated branches. In case 11 the pulmonary valve was unguarded and aortic overrided.
A small percentage of patients with this condition will die, including three who did not. However, in other cases, their lungs are so large that they cannot function as intended. Hence, the first treatment option should be a surgical procedure. The best outcome of the procedure would depend on the patient’s heart condition. The risk for pulmonary regurgitation is severe and will result in severe respiratory distress. A permanent repair of the pulmonary valve should be performed after a few weeks of the neonatal period.
This type of operation requires a relatively large number of reruns
Patients with minimal pulmonary stenosis generally follow the typical presentation of TOF. Occasionally, they have cyanotic spells or even cardiac failure. However, it is rare for the condition to lead to death. If there is a complication associated with the surgery, the patient is typically discharged home on postoperative day 34. This type of operation requires a relatively large amount of reoperation.
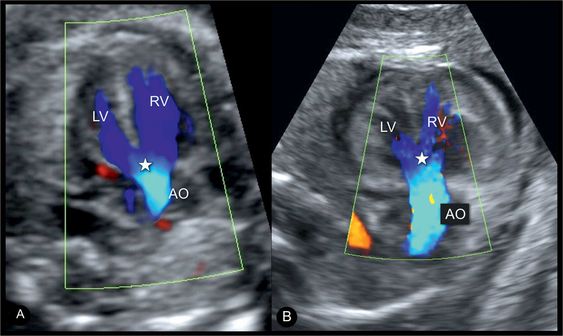
An MRI may also be necessary to diagnose the condition. The absence of pulmonary valve leaflets can also result in a dilated RV. In both cases, a CT scan can be helpful. A CT scan is an excellent way to visualize the pulmonary valve and its dilated branches. A CT scan was first described in 1847. The resulting image allows for a complete diagnosis of this disorder.
APVS cases were diagnosed within the observation period
In a recent study, 21 cases of APVS were diagnosed in an observation period. Sixteen of the cases were associated with a chromosomal anomaly. In addition to APVS, two cases had a patent DA and an intact ventricular septum. One patient had APVS without TOF. A third case was associated with an intact ventricular septum. The two cases were diagnosed before 24 weeks of gestation.
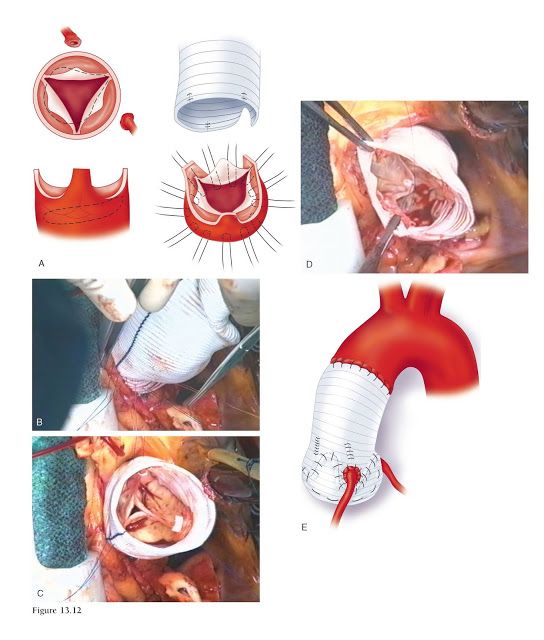
A new surgical technique can eliminate or reduce bronchial compression caused by the PA. It involves the correction of ToF, translocation of the PA anterior to the aorta, and plication of the PA. This new technique is reproducible and easy to perform. The new technique is the gold standard in APVS surgery. It may even eliminate the aortic valve. And the results can be quite dramatic.
The main independent risk factor for death after APVS
While there are few definitive studies on the surgical outcomes of APVS surgery, several other studies indicate that a patient’s preoperative ventilator dependence is a major risk factor for postoperative mortality. This fact should not be ignored, as it can impact the success rate of a surgical procedure. In fact, a recent study identified preoperative ventilator dependency as a major independent risk factor for mortality after APVS repair.
The first step in the treatment of APVS involves repair of the tof. The parietal band is transected through the tricuspid valve, releasing the obstruction in the right ventricular outflow tract. The ventricular septal defect is then closed with a knitted velour Dacron patch. Patent foramen ovale and atrial septal defect are closed using a continuous or interrupted suture technique.